The sensor would be embedded with an artificial lens during cataract surgery and would detect pressure changes. It was would integrate a low power radio chip to transmit measurement data.
“No one has ever put electronics inside the lens of the eye, so this is a little more radical,” said Karl Böhringer, a UW professor of electrical engineering and of bioengineering.
“We have shown this is possible in principle. If you can fit this sensor device into an intraocular lens implant during cataract surgery, it won’t require any further surgery for patients.”
There are two ways to check eye pressure, but both require a visit to the ophthalmologist.
At most, patients at risk for glaucoma may only get their pressure checked several times a year, said Tueng Shen, a collaborator and UW professor of ophthalmology.
But if ophthalmologists could insert a pressure monitoring system in the eye with an artificial lens during cataract surgery that could save patients from a second surgery and essentially make their replacement lens “smarter” and more functional.
“The implementation of the monitoring device has to be well-suited clinically and must be designed to be simple and reliable,” Shen said. “We want every surgeon who does cataract surgeries to be able to use this.”
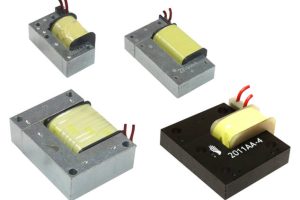
The UW engineering team has built a prototype that uses radio frequency for wireless power and data transfer. A thin, circular antenna spans the perimeter of the device – roughly tracing a person’s iris – and harnesses enough energy from the surrounding field to power a small pressure sensor chip.
The chip communicates with a close-by receiver about any shifts in frequency, which signify a change in pressure. Actual pressure is then calculated and those changes are tracked and recorded in real-time.
The chip’s processing mechanism is actually very simple, leaving the computational heavy lifting to the nearby receiver, which could be a handheld device or possibly built into a smartphone, Böhringer said.
The current prototype is larger than it would need to be to fit into an artificial lens, but the research team is confident it can be downscaled through more engineering.
The team is working on downscaling the prototype to be tested in an actual artificial lens. Designing a final product that’s affordable for patients is the ultimate goal, researchers said.
“I think if the cost is reasonable and if the new device offers information that’s not measureable by current technology, patients and surgeons would be really eager to adopt it,” Shen said.
The research was funded by the Coulter Foundation and the UW. Buddy Ratner, a UW professor of bioengineering and of chemical engineering, and Felix Simonovsky, a UW bioengineering research scientist, also contributed to this work.
The University of Washington researchers recently published their results in the Journal of Micromechanics and Microengineering and filed patents on an initial prototype of the pressure-monitoring device.
 Electronics Weekly Electronics Design & Components Tech News
Electronics Weekly Electronics Design & Components Tech News